Talking about mental health at RSECon22
8 November 2022
By Dave Horsfall, Software Sustainability Institute Fellow.
In early September I was given a fantastic opportunity to speak about mental health in a plenary slot at the annual conference for Research Software Engineering in the UK.
I was awarded an SSI fellowship in 2021 to advocate and raise awareness of mental health in the research software community. Over the last 18 months, I’ve spoken to many groups of RSEs, but this was by far the largest. I really enjoyed the session and received lots of feedback and engagement afterwards. My presentation is available to watch on the RSE Society YouTube channel.
I use interactive presentation software for my talks, which allows the audience to give real-time anonymous feedback and responses to questions. There are lots of interesting results and comments from the audience relating to mental health and causes of stress whilst working as an RSE. You can download a copy of the slides and see all the audience responses here.
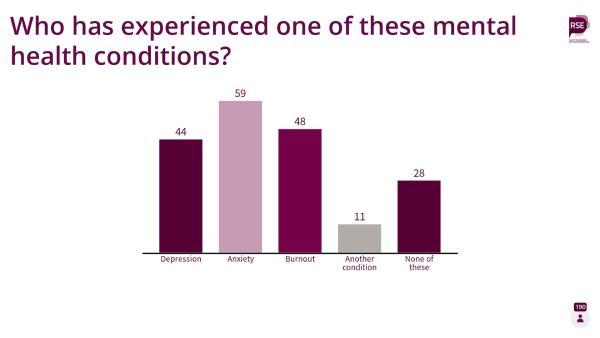
The key takeaway point from the session that I want to highlight is that from 190 responses, 162 people (85%) indicated they assessed themselves as having experience of a mental health condition. I think this shows we need to be talking a lot more about mental health, and creating spaces where people can talk freely about their experiences, without judgement.
During my talk, I also launched a national mental health survey for research software engineers. The aim is to capture a snapshot of mental health within the research software engineering community and explore the steps that might be taken to improve things. If you work as a Research Software Engineer, please complete the survey. It will take around 6 to 12 minutes, depending on your answers. I’m targeting responses from inside the UK, however results from outside the UK will be saved and included in the final report.
Throughout the presentation, the audience was able to ask questions using Slido. There were many great questions but I wasn’t able to answer them due to time constraints. Additionally, it is important for me to be clear that I'm not a trained mental health professional. It is sometimes difficult for me to give answers to questions on this topic on-the-fly. With help from Anika Cawthorn, a mental health advocate in the community, I want to give responses to all the fantastic questions. Below is the list of audience questions along with our best attempt at an answer.
Do you have any suggestions for dealing with the ‘risk’ of raising a mental health issue in a job interview - or do you think best not to raise at this stage?
Firstly, it is important to clarify that you don’t have any legal obligation to disclose a mental health problem during a job interview. If an employer asks you any type of health question before making you a job offer, you can report this to the Equality Advice & Support Service (EASS).
Whether or not you should disclose a mental health issue is of course a different question, and I don’t think there is a right or wrong approach to this. It depends on the individual, the type of role and nature of the relationship you want to have with the employer.
For example, at this stage in my career I wouldn’t want to work for an employer who wasn’t supportive of mental health, or in a team that culturally wasn’t open to discussions about mental health. You may wish to be upfront with an employer and disclose a condition before an interview. Alternatively, you might want to wait until after you have been made an offer, and then discuss things to decide whether or not to accept the position. If I was to discuss a mental health issue with a potential employer, then it would be important to be prepared for the conversation:
- Generally you would only disclose conditions that could affect your role, and which may warrant a consideration of adjustments.
- Be clear about the problems that you are having, and how these will impact your ability to do your job.
- Make sure it is a two-way conversation and ask what adjustments could be made for you at work.
- Be clear about confidentiality. Make sure you understand what will happen next within the organisation. Ask who will be notified about your discussion, and be clear to the employer if you’d like to be open with the wider team about your mental health issue. It's perhaps also good to be clear with your current employer whether or not you want info to be passed on if they write a reference. Some people might try to give helpful advice on how they helped someone to succeed and unknowingly disclose confidential information.
- You may want to explore the culture of the team and organisation. You could enquire what training your line manager has in order to support you, and what other means of support exist. For example, Mental Health First Aiders (MHFA), Employee Assistance Programmes (EAP), well-being champions, subscriptions to online support tools. etc
Being overwhelmed with too many tasks seems to be a very common problem. Any specific tips?
Signs you’re overwhelmed at work:
- You always feel helpless, i.e. you feel like you’ve lost control and you have no direction in your professional life.
- Work is constantly on your mind, i.e. your job dominates your every waking (and sleeping) thought.
- You have a “Restless mind”, i.e. you change frequently between different tasks and thoughts without really making progress on anything.
- Sleep is difficult, i.e. you’re up at all hours with anxiety and dread about what the next day will bring.
- You’re always exhausted i.e. you can’t escape your exhaustion and perform poorly at work, develop a short fuse, and lose your drive to succeed.
- Your eating habits change, i.e. dramatic loss of appetite, or binge eating.
- You get sick a lot, including headaches, ulcers, stomach or chest pains, fatigue.
- You feel increasingly hostile and pessimistic, i.e. your daily outlook casts a dark shadow over everything.
How to stop feeling overwhelmed at work:
- Understand the things that trigger feeling overwhelmed.
- Unload everything in your mind.
- Use Parkinson’s Law to your advantage.
- Set appropriate boundaries.
- Define the things you can and cannot change.
- Delegate and ask for help.
- Think about your stress bucket.
For more details on these points, please read this article by Stephen Altrogge.
What are you supposed to do if you have a more stigmatised mental health condition than depression or anxiety?
I remember I tried to answer this one at the end of my talk and didn’t do a very good job.
In terms of your employment, regardless of the condition, if your mental health difficulty is long-lasting and interferes with your ability to perform normal daily activities you are protected by the Equality Act, which requires appropriate reasonable adjustments to be put in place.
Public stigma involves the negative or discriminatory attitudes that others have about mental illness. During my reading about this, I’ve found several articles that indicate the most stigmatised mental illnesses are schizophrenia, dissociative identity disorder, and borderline personality disorder (BPD).
Here are seven things people can do to reduce stigma:
- Know the facts. Educate yourself about mental illness.
- Be aware of your attitudes and behaviour. Examine your own judgmental thinking that is reinforced by upbringing and society.
- Choose your words carefully. The way we speak can affect the attitudes of others.
- Educate others. Pass on facts and positive attitudes; challenge myths and stereotypes.
- Focus on the positive. Mental illness is only part of anyone's larger picture.
- Support people. Treat everyone with dignity and respect; offer support and encouragement.
- Be inclusive. It's against the law to deny jobs or services to anyone with mental health issues.
Depression and anxiety are the two most common mental health issues. The relationship between the prevalence of a mental illness, rates of disclosure and stigma is complex. Anika made the comment that because anxiety and depression are more common, some people think that they know what you are going through when you have this illness, and she doesn’t think that is true either. Illness, independent of label, should be recognised as such and be supported, no matter what it is. If there are adjustments available then it shouldn’t matter what the condition is. Perhaps a good way of approaching this, if the line manager is not equipped, could be to go through occupational health or some other independent service. Anika has previously been in this situation where her GP wrote a small recommendation on how to deal with the health situation. Another option could be a workplace action plan to list how the illness manifests and what actions could be helpful when health deteriorates.
Widespread problems require collective solutions. Can we suggest to people that joining a Trade Union is good for their and everyone's mental health?
We're stronger together. The University and College Union (UCU) is the largest trade union for academics, lecturers, trainers, researchers and academic-related staff working in further and higher education throughout the UK. They have a dedicated toolkit for supporting members with mental health conditions and issues.
What ways can you approach talking to supervisors about chronic mental health disorders without it negatively affecting their perception of you and your actions?
If you are struggling or you are managing a chronic mental health disorder, it is good to talk about this with someone at work, ideally your supervisor. It might feel hard but if you can make them aware you are having difficulties, they can try to help, putting measures in place to support you now and in the future. If your mental health difficulty is long-lasting and interferes with your ability to perform normal daily activities you are protected by the Equality Act, which requires appropriate reasonable adjustments to be put in place.
Training on mental health is increasing and new resources are becoming available to line managers, but there is still a problem with awareness so a facilitating line manager is not a given. It is completely understandable you might be concerned about starting a conversation with your supervisor, especially if the subject of mental health has never been discussed within the team before, and you are unsure what the reaction will be. However, if you can start the conversation then it might actually allow the line manager to understand what you are going through. It shouldn’t be the case that you need to educate your line manager about your mental health condition, but explaining things from your perspective can really help. Quite often people assume that mental illness is “just in the mind” whereas it can have a whole host of physical problems and describing those might make the struggles more obvious. Anika has at times taken illustrations such as tinnitus noises and visualisations of scintillating scotomas to meetings and found that explaining those helped, but is of course no guarantee.
If you are concerned about the initial conversation with your supervisor then you might want to start by calling your Employee Assistance Program (EAP) and talking to them about what they would advise in terms of adjustments and how to approach the conversation with the line manager. Alternatively, you could contact me to discreetly propose a mental health talk to your team. It may help open the conversation around mental health, and allow you to gauge the reaction from your team.
Mental health issues at work are a structural issue as well as an individual issue. How can we help positive change in the workplace to better support employees?
Firstly, we need to talk more about it and share stories where people have been helped and supported. I personally think that calling out problems is a good start, but when it comes to help, people can get paralysed by the thought of doing something wrong. Meaningful cultural change is very difficult, but discussing suggestions on how things could work and what has been helpful to individuals is tremendously important in this context. This could lead to new policy, which would drive more awareness, and standardise mental health support across the RSE community.
How do you know when you have imposter syndrome and when you are legitimately lacking in capability?
Good question! I'm not sure I’ve thought much about that before. Being hired for a job means that you’ve already met the required level, and that others agree with that judgement. People tend not to be a perfect fit for a role when they start, and the expectation is that you grow and develop in the relevant areas over time through support and training.
These are perhaps a couple of ways to explore this:
- Seek feedback from your supervisor - they will be able to give you a sense of your overall performance. If your supervisor is positive you can be pretty sure that you’re doing a good job. Get feedback on the things you do well, but if they identify areas where you need to improve then hopefully they can support you through that process. Remember, if you identify areas for improvement, this doesn’t mean you are lacking in capability.
- Use your self-awareness as an advantage - the key here is to find the balance between growth and self-awareness without criticising yourself too harshly. Everyone makes mistakes, and that’s ok. Mistakes allow for reflection. The key is to see them as teachable moments.
- Have a look at the Coding Confessions sessions and blogs to see that mistakes and errors happen to everyone.
Any tips on how a team culture can foster mental health awareness?
Employers and managers must create an organisational culture that de-stigmatises mental health issues, while normalising and encouraging help-seeking behaviours. This involves:
- Having a mental health policy.
- Promoting awareness.
- Fostering a supportive culture.
- Creating open channels of communication.
- Promoting healthy behaviours at work.
- Providing accessible resources.
- Leading from the front.
I’m building a network in the RSE community to work on resources that will help teams achieve this culture. Please join the mailing list to get involved or stay updated.
What institutional changes are needed to control workload?
This is difficult to answer. Institutional problems around workload culture are widespread and complex. Calm Business has an article outlining a two-pronged approach to better workload management. They suggest most workload issues come down to organisational problems, like the following:
- Managers assigning too much work.
- Distracting, interruption-heavy work environment.
- Lack of accommodations or support for neurodiverse workers.
- Limited workplace flexibility for employees.
- Not enough company resources to spread out the workload.
- Poor communication between leaders and employees.
- Not offering employees enough training.
- Not giving employees tools to manage their work volume and mental health.
The article then proposes a framework on how managers and supervisors can improve workload management, and also how we can individually manage our own workload to support mental health.
With Covid on top of normal illnesses, most of us are already getting "flagged" for taking too much sick leave. Should burnout leave = sick leave?
Yes, burnout leave is sick leave. With any sickness related absence, you're legally entitled to sick pay however, if you’re repeatedly absent from work then you may pass a threshold where your pay starts to decrease. Unfortunately, this can cause significant additional stress, making the problem worse.
If the underlying cause of the burnout is not going away then it is important to start discussions with your employer about actions and adjustments that might help. This is where managers need to be proactive, identifying when team members are struggling and putting preventative measures in place early. Giving a few days off, or managing a slightly reducing workload is far better than having team members who are on prolonged and unpredictable sick leave due to stress and burnout.
Any comments on how to balance taking breaks to mitigate burnout vs fixed term contracts?
I’m sorry if I’ve misunderstood your question.
Perhaps something around workload agreements and depending on the state of the person’s health then also reasonable adjustments? Those could include regular breaks, e.g. starting on 80% to allow recovery. Nobody should be disadvantaged because of their state of health or being affected more by stress.
Self care is good but not a solution for external factors. How should leaders be changing environments so we don't have to do yoga?
There is no “one size fits all” and individual solutions need to be found. We all have factors of stress in our lives, and good stress is vital for a healthy life. We all need to develop our own unique set of strategies that help manage stress. Some people enjoy yoga and use that as a way of clearing their mind. The problem I sometimes see is that people expect others to know what they need, but that is very hard to guess because we are not all the same. Employers do have a duty of care and there are different ways of starting the conversation with them. I think the first step is for RSE leaders to engage the community and understand what factors in the environment cause stress and mental health problems. Perhaps the results from my mental health survey can help start that conversation?
Where can we find more information about mental health first aid?
Mental health first aid is to help people in crisis access the support they need. They might not be aware they need help, or they may struggle to assess their support options themselves. It’s about signposting people to the right place. Mental health is health, just like physical health.
Mental Health First Aid (MHFA) England is a social enterprise that offers expert guidance and training to support mental health in the workplace. In a nutshell a Mental Health First Aider aims to support someone in a situation of deteriorated mental well-being to find the help that is best suited to their situation. To be clear though MHFAs are trained volunteers, not counsellors or psychiatrists and as such will not provide a diagnosis.
If you would like more information about mental health first aid within the RSE community, please contact Anika Cawthorn. An initiative to train more mental health first aiders in the community is being actively developed. Join the mailing list to keep up to date with developments.
In the private sector, overworking will always get you ahead, can we make that not the case in RSE and how?
This is something that I have thought about a lot. You’re right that the private sector is known for a culture of overworking. However, academia also has a very poor work culture. The RSE ecosystem is still emerging which gives us a unique opportunity to create a different culture and establish healthy working patterns and sustainable career opportunities. This culture can be driven by the community, and standardised with new policy. We need to do this together, so please join the mailing list to get involved.
I've had students work for me. Sometimes they have expectations and even desires to work longer hours than I do and their contracts cover. Should I discourage them?
Yes, I believe you should discourage your team from working significantly longer hours than specified in their contracts. It doesn’t help them, and it perpetuates the culture of overwork. Other students see it, and think they need to do the same to have the same opportunities. Some students are just really passionate, and love working. However, you can be vocal about healthy working patterns during team meetings, and regularly define your expectations.
It is important to recognise that we live in a world of flexible and hybrid working. It might be that some people prefer to work in the afternoons and evenings, or maybe they like to start work very early and finish early. If someone is always in the office in the evening, it doesn’t necessarily mean they are working long hours. Again, having open and clear communication about this within your team is important. Make sure you understand when people tend to work, and make sure everyone else in the team knows this too. Encourage everyone to keep to their hours, and invite them to speak with you if they feel they can’t do this due to high workload.
How to challenge uncaring Profs?
This is a difficult one because the differences between RSEs and postdocs aren’t always made clear, and there is huge variation in the working environments for RSEs across institutions. Try to be as clear as possible that RSEs are not a short term replacement for a postdoc, rather someone skilled in software engineering. One option for centralised RSE teams could be to set “working rules” as a group and a prof would need to agree with this before work begins. These rules could include a policy on working hours and if things go pear-shaped one can point back to the rules that were set out at the beginning. This is more difficult for embedded RSEs, however, it is fairly common for institutions to have a Supervision Agreement which defines expectations for working arrangements from both sides before a relationship starts. Good communication, and clearly defining expectations is really important. If the relationship deteriorates, issues could be raised with the head of the group or HR.
Thank you so much for doing this talk, it's so helpful to understand that I am not alone with my mental illness!
Thank you. It means a lot that you found it helpful, and that it highlighted the prevalence of mental health issues in the community. From 190 responses, 162 people (85%) indicated they assess themselves as having experience of some type of mental health condition. I think this shows we need to be talking a lot more about mental health, and putting more resources into supporting our workforce.
How can we support managers to look after the wellbeing of their staff?
Training and more resources. I think it also has to do with creating a positive space around mental health. It should not be seen as a tick-box exercise that line managers have to do, rather something that they see as a helpful addition and want to do to support their staff better. Unfortunately, lack of priority in this area from managers is probably impacted by the ever increasing workloads, and simply not having enough time for it. I’m building a network in the RSE community to work on resources that will help managers improve support for mental health in their teams. Please join the mailing list to get involved or stay updated.
Mental health is not always driven by work.
This is a great point, there are many factors outside work that influence our mental health. It is important to accept that work probably shouldn’t be the most important thing in our lives, and that people can have complicated and stressful responsibilities in their personal lives.
However, if you have factors outside work that are impacting your performance at work, it is important to communicate these with your employer so that they are aware of the situation and help support you through appropriate adjustments.
How can we reduce unconscious bias within the community?
One of the key aims of my SSI fellowship is to reduce the stigma associated with mental health, which can lead to unconscious bias. I’ve tried to achieve this by talking and raising awareness in the community. The more people see that we as a community take mental health and well-being seriously, the more will join in. The more we help each other understand individual viewpoints, the more we can do to support each other. Going back to one of the previous questions, I think we need to start sharing stories about helpful and unhelpful behaviours that then create transparency for others. Additionally, we can be more effective allies for mental health by challenging unhealthy cultures and behaviour in the workplace.

